Can AI Fix South Africa’s Crumbling Healthcare System Without New Risks?
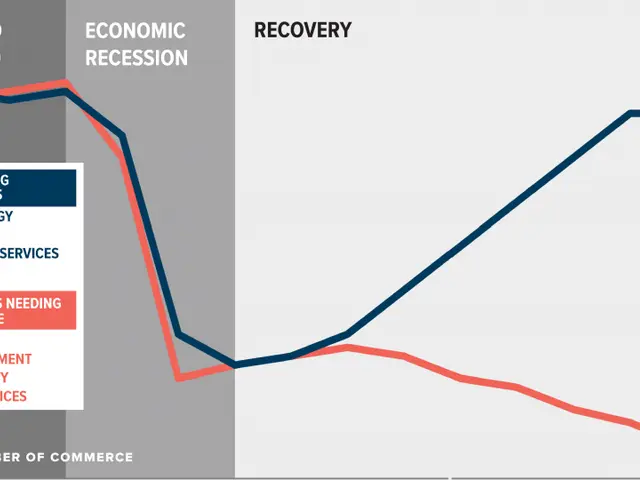
South Africa’s healthcare system is under severe strain, with rising patient demands, crumbling infrastructure, and a critical shortage of medical staff. These challenges have fuelled a sharp increase in medical negligence claims, costing the country over R4.12 billion in payouts between 2020 and 2023 alone. Now, artificial intelligence (AI) is emerging as a potential solution—but its adoption brings both promise and new legal complexities.
Medical negligence in South Africa is governed by delict law, which requires proof of a duty of care, its breach, causation, and patient harm. Between 2014 and 2020, claims surged by an average of 23% annually, reflecting systemic failures in public health services. AI could ease some pressures by improving diagnostic accuracy, detecting early-stage diseases, and optimising resource use. Yet its integration also introduces risks, from algorithmic errors to data privacy breaches and unclear liability when systems fail.
To manage these challenges, experts argue for a robust regulatory framework. The EU AI Act, Medical Device Regulation (MDR), and In Vitro Diagnostic Regulation (IVDR) offer models for risk management, transparency, and data quality. South Africa could adapt these standards by aligning them with local laws like the National Health Act, streamlining technical documentation, and prioritising interoperable health data systems. National guidelines on AI risk classification and patient transparency would further strengthen trust and innovation. The goal is clear: AI must support, not replace, clinical decision-making. A well-regulated approach could help mitigate risks while maximising benefits for a struggling healthcare system.
South Africa’s healthcare crisis demands urgent solutions, and AI presents a double-edged opportunity. If implemented with strong legal safeguards, it could enhance diagnostics and efficiency. Without proper oversight, however, it risks exacerbating existing problems—from malpractice claims to patient safety concerns. The path forward requires balancing innovation with accountability within the country’s unique medico-legal landscape.